Today’s post is a bit more morbid than my usual topics, but I think it’s something that is very important to think about for everyone, no matter how young or how healthy you might be.
The old saying goes “the only two certain things in life are death and taxes.” Whether we like it or not, we are all going to die one day. I think it only makes sense that we give a little bit of thought to how we would like to die, and then (just as important!) communicate our wishes to our families.
The large majority of people would prefer to die in their own homes, but in modern America, the majority of people die in the hospital, usually with multiple invasive tubes and iv lines inserted into their bodies.
Why does this happen?
The reasons are many, but here are two important ones. First, most people don’t really want to think about the end of their lives, and even if they do, they don’t want to upset their spouses or families by talking about their wishes. Second, once someone is very sick with a terminal illness and can no longer communicate their wishes, the usual instinct of their family members and doctors is to err on the side of intervening and treating the illness.
So, people who would have rather died peacefully in their own beds end up being transported to the hospital, kept in the ICU for 2 weeks, had breathing and feeding tubes placed, and then die in the hospital after racking up 6 figures in pointless medical bills.
If you would want to have everything done to keep you alive in that situation, you have every right to that treatment! But most people with a terminal illness (meaning that your doctor believes you have a non-curable disease and likely will die within 6 months) do not want heroic efforts to keep them alive. Most people in that situation are much more concerned with staying comfortable and being able to appreciate their last few months, weeks, and days with their loved ones.
For patients with terminal illnesses, Hospice care can be a great blessing. Hospice is an organization that provides counseling, comfort care, and nursing for terminally ill patients at home or in the hospital. The goal of Hospice is not to cure the disease but rather to keep each patient as comfortable, alert, and interactive as possible through their last months.
Although the mission of Hospice is not to prolong life, numerous research studies have shown that patients in Hospice actually do live longer (and with a better quality of life) than patients who “want everything done.”
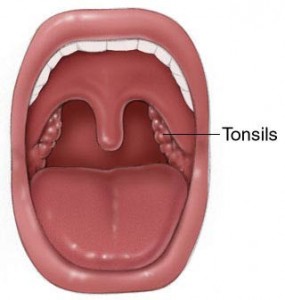
I am fortunate to be in a specialty without very many terminally ill patients, but I do see some patients with head and neck cancers who cannot be cured with surgery, radiation, or chemotherapy. For these unfortunate patients, I strongly urge them to think about Hospice.
But even before, everyone should think about their end of life wishes. Particularly so if they are diagnosed with a life threatening illness, such as cancer, heart disease, or COPD. The time to think about it is when you feel well and have your wits, not when you are on death’s door.
The state of Texas has a very good information page that will walk you through the decisions you need to think about. Link to webpage here. It provides templates for various legal documents that can record your wishes for when you are unable to communicate them. The PDF file at the bottom of that page called “Thinking Ahead: My Way, My Choice, My Life at the End” is excellent.
Every person will have to decide for themselves if they want to draft an official advanced directive and medical power of attorney to ensure their wishes are followed. Most of the time, doctors will ask your family what you would want done if you can’t communicate your wishes. As long as you’ve discussed your wishes with your family (and they are all on the same page), an official advanced directive may not be necessary. But in my opinion, you’re better safe than sorry to put it down in writing. That way, if your family is very emotional and might want to be more aggressive with your treatment, your wishes will be there in writing for everyone to see.