Tonsillectomy and adenoidectomy (T+A) is one of the most common surgeries performed in the United States each year. The surgery is performed while the patient is completely asleep under general anesthesia. Many times, patients are able to go home safely the same day as their surgery, but in certain cases they may need to stay overnight in the hospital for monitoring.
What is T+A surgery?
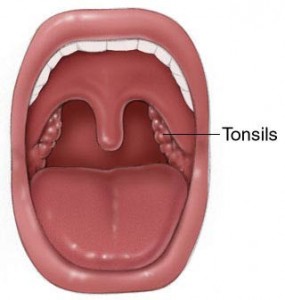
The surgery involves removal of the two tonsils which are visible in the back of your mouth as well as the adenoids, which live in the back of your nose behind the soft palate (roof of your mouth). In teenagers and adults, frequently the adenoids do not need to be removed because they have already shrunken away completely.
Why do people need T+A surgery?
The two most common reasons are 1. recurrent or chronic throat infections (aka strep throat, tonsillitis, or pharyngitis) and 2. very large tonsils and adenoids which cause breathing problems. There are other less common reasons including tonsillar or peritonsillar abscess, recurrent tonsil stones, asymmetric size of the tonsils with suspicion of a tumor.
Recurrent tonsillitis is defined as 6-7 tonsil infections/strep throat in 1 year, 5 infections per year for 2 years in a row, or 3 infections per year for 3 years in a row. Chronic tonsillitis is an infection which does not completely go away after at least 3 months despite antibiotics.
Very large tonsils and adenoids can cause narrowing of the airway which can cause breathing problems while asleep. This problem is called obstructive sleep apnea. Typical signs in children include choking/gasping spells while asleep, loud snoring with periods of not breathing, bed wetting, behavioral problems, and attention problems during the day. In most children, T+A surgery will dramatically improve their breathing while asleep. Snoring alone without evidence of true sleep apnea is generally not a reason to need T+A surgery. In uncertain cases, a sleep study can be very useful to determine who does and does not need surgery or other treatment.
How is the surgery performed?
After the patient is asleep under anesthesia, the surgery is all done through the mouth with no skin incisions. I use an electric knife which is able to cut tissue and cauterize bleeding at the same time to remove the tonsils. For the adenoids, I usually use a device to burn the tissue away (rarely I need to actually cut the tissue out). The surgery usually takes around 20-30 minutes, not including going to sleep and waking up.
What are the possible risks of surgery?
T+A surgery is very safe. The risk of serious or life threatening problems is extraordinarily rare (as in “struck by lightning twice” rare) and would usually be caused by bad reactions to anesthesia. The anesthesiologists I work with are very experienced with these surgeries and with patients of all ages.
The most common risk after T+A surgery is bleeding from the mouth. This occurs in about 3% of patients on average. Bleeding is most likely to happen 7-10 days after surgery. The best way to minimize risk of bleeding is to strictly stay on the correct diet and activity restrictions (see below). A small amount of blood mixed in the saliva is normal for a day or two after surgery. If true bleeding occurs, go to the nearest emergency room right away so that the problem can be addressed. Almost always, bleeding can be stopped without much difficulty. Severe bleeding is very rare.
Other uncommon risks include damage to the lips, gums, or teeth. Also patients will occasionally notice that liquids go backwards into the back of their nose while swallowing during the first few days after surgery. This will almost always resolve with a little time.
After removal of the adenoids, nasal congestion, bad breath, and neck stiffness are all common complaints during the healing period.
What should you expect after surgery?
Unfortunately, T+A surgery is relatively painful. The average patient will have 1 week of a miserable sore throat after surgery and then a second week of slowly improving sore throat. Some patients sail through, and some will be miserable for a full 2 weeks. On average, the older the patient, the worse pain they will have after tonsillectomy. I prescribe plenty of liquid pain medication for patients after this surgery, so don’t be afraid to take it. I also prescribe one week of liquid antibiotic to take after surgery (amoxicillin unless the patient is allergic).
Some patients will be sick to their stomach during the first 24 hours after surgery, usually because of lingering anesthesia effects. If you continue to have significant nausea or vomiting more than 24 hours after surgery, it might be a side effect of your pain medication. If this happens, call my office and I can change your prescription.
It is very important that patients strictly follow a soft and liquid diet for a full 2 weeks after surgery. Soft diet means that you can only eat things that you don’t have to chew up before swallowing. This would include jello, pudding, mashed potatoes, scrambled eggs, ice cream, popsicles, etc. You cannot eat hamburgers, chips, fries, chicken tenders, pizza, cereal, or anything else solid that requires chewing. If your child does not want to eat much it is ok. However, it is extremely important that your child drinks lots of fluids. Getting dehydrated will start a vicious cycle of worse throat pain, increased risk of bleeding, and more difficulty swallowing. Your child has to drink fluids, it is not a choice.
Patients should avoid any running, heavy lifting over 10 pounds, or strenuous play for 2 weeks after surgery. I will give a school excuse for up to 2 weeks out of school. If your child is feeling well and off prescription pain medication before 2 weeks, he or she can return to school but must stick to the soft/liquid diet and stay out of gym class until the 2 weeks is up. Adult patients can return to work when they want, but must avoid strenuous activity for 2 weeks and must stay on the proper diet. I would strongly urge any adult patients to have stopped taking prescription pain medication for at least 24 hours before returning to work.
If you look in your mouth or your child’s mouth during the healing period, you will see white or yellow patches where the tonsils were removed. These are called exudates and are normal.
Ear pain is normal after T+A surgery, and is caused by referred pain from the throat.
I like to see patients back in the office 2-3 weeks after surgery to make sure things have healed properly.