And I’m back! My wife and I had a wonderful few weeks getting married in Austin and then experiencing the amazing islands of Kauai and the Big Island in Hawaii earlier this month.
Today I’m going to talk about a book I recently read on the topic of chronic cough (defined as a cough which lasts longer than 8 weeks). The author is a famous otolaryngologist, Dr. Jamie Koufman, who has been treating patients with throat, swallowing, and voice problems for the past 30 years or so. She was formerly faculty at the Wake Forest University department of ENT and more recently has set up a practice dedicated to throat disorders in New York City, the Voice Institute of New York. She is well known as a world expert (probably THE expert) on airway reflux and cough.
Link to Amazon page HERE.
The book is fairly compact and well organized. The book is aimed primarily at people with non-pulmonary (i.e. not caused by lung problems or smoking) chronic cough. Most of these people have seen many doctors in several different specialties (ENT, GI, pulmonary typically) without relief. Dr. Koufman makes the point in the book (and I agree) that the problem of non-pulmonary chronic cough overlaps the areas of these 3 specialties and to be treated effectively needs a more comprehensive approach.
In her experience of seeing many thousands of patients with this problem, Dr. Koufman has concluded that the vast majority of non-pulmonary chronic cough patients owe their problem to one or both of the following underlying causes:
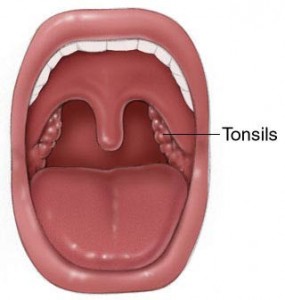
1. Airway Reflux (stomach acid/juice which comes backwards into the throat, airway, and lungs)
2. Postviral Vagal Neuropathy a.k.a. Neuropathic cough (chronic inflammation/dysfunction of the vagus nerve following a cold or other viral upper respiratory infection)
The large majority of the book is dedicated to explaining the underlying mechanisms for these problems, how they are diagnosed, and how they are treated.
She provides helpful short surveys to determine with >90% accuracy if you have one or both of these underlying problems.
She also describes her recommendations for treating the problem. For reflux, she believes that reflux can be cured by dietary and lifestyle changes. Her recommendations are summarized in this book and are laid out in more detail in her other book, Dropping Acid: The Reflux Diet Cookbook and Cure. She also discusses medical treatment of reflux with medications like proton pump inhibitors (ex. Prilosec, Nexium, Protonix, others) and H2 blockers (Zantac, Pepcid, Tagamet). She is quite cautious with medications, especially the PPIs and uses them sparingly.
For neurogenic cough, she describes her usual medicines (amitriptyline, gabapentin, tramadol), which are similar to those outlined in my post on chronic cough from a few months ago.
I found the book to be personally useful for several reasons. One is providing a more “big picture” look at chronic cough, reflux, and vagal neuropathy. Another is the idea that reflux can be cured by dietary changes and that the standard treatment with long term proton pump inhibitors is only masking symptoms and can be potentially harmful. I plan to incorporate the information in this book to better treat the many patients I see with chronic cough and/or reflux.
For patients, the writing is overall pretty clear and understandable. There are a lot of medical terms, but there is an extensive glossary at the end of the book to help you understand them. In the Kindle edition which I read, all the medical terms are linked directly to the glossary.
I would encourage anyone with chronic cough, acid reflux, or asthma to read and understand this book. You can purchase it HERE.